Today I would like to present a patient success story in which we combined physical therapy with massage therapy to accelerate the rehab process from a shoulder injury. We will go over the patient’s presentation, my assessment of what was going on, and how we got her better. (I changed the patient’s name for the sake of privacy.)
Patient presentation:
History:
Our patient is Linda, a 72 year old female who appears much younger than her age who is generally active with walking, yoga, and occasional golf, and is generally very health conscious. She began having pain on the outside of her left shoulder about 2 months prior to coming to me for physical therapy. She could not recall a specific injury but noted that the pain came on gradually and had progressively been getting worse to the point where simple reaching, lifting and carrying tasks were now painful. She had already gone to another physical therapy clinic for about 2 weeks prior to coming to me, which actually made her symptoms worse. When I asked her what they had her doing she said they were doing shoulder stretching exercises on a ball and some rubberband strengthening exercises. When the stretches were only making her shoulder worse and her therapist was not adjusting her program she knew it was time to try something else. Because she tried physical therapy and it failed to improve her situation, her surgeon was recommending surgery for a possible rotator cuff tear that showed up on her MRI. Linda wanted to avoid surgery if at all possible and was willing to give physical therapy another try, but with me this time. Her goal was to eliminate her pain and return to yoga and occasional golf without pain or limitation.
Physical exam:
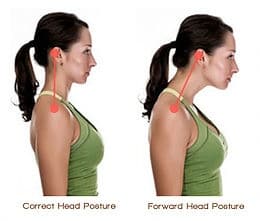
In my physical exam of Linda, it was clear that posture was a big contributor to her problem. She displayed forward shoulder posture on both sides, forward head posture, and winging of her shoulder blades (See pictures for examples of these impairments).
When I watched her walk and perform normal reaching tasks, I could see that she had very little motion coming from her thoracic spine (upper back) or shoulder blades contributing to shoulder motion, meaning that the shoulder joint was contributing a disproportionate amount of movement when compared to these other areas. Linda was painful and weak with reaching forward and to the side, and she had weak shoulder blade and rotator cuff muscles. Clinical tests for a rotator cuff tear were negative while tests for shoulder impingement were positive (If you don’t know what shoulder impingement is I’ll explain that later).
My assessment:
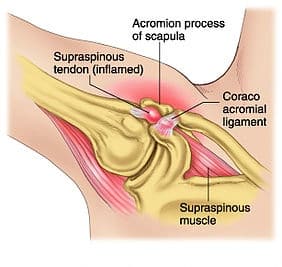
In my professional opinion, I felt that Linda had subacromial impingement. This means that her rotator cuff tendon was being pinched by the acromion process (bone at the tip of the shoulder) every time she raised her arm. Please see the pictures to get a more clear picture of what is happening with this. The reason this was happening was due to poor posture at rest and lack of thoracic spine and shoulder blade movement during raising of the arms. Linda had tightness in her thoracic spine combined with tightness of certain muscles and weakness of others that prevented her thoracic spine and shoulder blade from contributing their fair share of movement during reaching tasks. This lead to pinching of her rotator cuff tendon under the acromion every time she raised her arm, which lead to tissue inflammation and pain over time.
What we did:
After I performed my evaluation I started treating linda with manual therapy, education, and light exercise on day one. I did some targeted soft tissue work to release tight muscles that were specifically limiting her posture and ability to move the shoulder blade, and I did some work to loosen the joints in her thoracic spine. Immediately she was able to raise her left arm with almost no pain and with greater range of motion. I educated her on her condition and gave her some simple exercises to perform self massage to tight muscles and work on posture. This helped reduce pain with reaching by about 50% within a week.
After about 2 weeks of physical therapy we had been progressing strength exercise and including movement re-education to teach her how to move correctly, but it was evident that muscular tightness was still a huge limiting factor in her progression. I wanted her to get more work done to address those tight soft tissues, so I referred her to my preferred massage therapist, with some instructions to the massage therapist as to what areas to focus on. Linda needed this because in physical therapy I needed to split time between massage, movement re-education, and strengthening to address all aspects of her problem, but she simply needed more time dedicated to loosening those tight muscles. Massage therapy was the answer. They could spend an hour or more dedicated to loosening tight muscles. Once she started getting massages once a week, her rehab accelerated dramatically. Getting her soft tissues released allowed us to progress her movement re-education and strength exercise much faster and she reached her goals of returning to yoga and golf without pain in 2-3
weeks.
Conclusion:
Linda’s case is a great demonstration of 2 things: 1) It is important to not only treat the site of injury, but to address surrounding areas that may be contributing to faulty movements or positions that may ultimately be causing the injury. Linda’s previous physical therapist failed to do this and as a result did not address the root causes of her problem; 2) The positive effects of physical therapy can be magnified or accelerated when combined with other services when appropriate. In Linda’s case it was massage therapy to release restricted muscles of the shoulder and shoulder blade. But services from other professionals such as acupuncturists, chiropractors, nutritionists, naturopaths, trainers, golf instructors, and many more can complement physical physical therapy to help you get out of pain and back doing the things you love to do. At The Doctors of Physical Therapy we treat the person in a holistic way and are not afraid to reach out to other professionals when it is in the best interest of the patient.